Breast Reconstruction
Breast Reconstruction Procedures
IF YOU ARE CONSIDERING BREAST RECONSTRUCTION…
Reconstruction of a breast that has been removed due to cancer or other disease is one of the most rewarding surgical procedures available today. New medical techniques and devices have made it possible for surgeons to create a breast that can come close in form and appearance to matching a natural breast. Frequently, reconstruction is possible immediately following breast removal (mastectomy), so the patient wakes up with a breast mound already in place, having been spared the experience of seeing herself with no breast at all.
But bear in mind, post-mastectomy breast reconstruction is not a simple procedure. There are often many options to consider as you and your doctor explore what’s best for you.
This information will give you a basic understanding of the procedure, when it’s appropriate, how it’s done, and what results you can expect. It can’t answer all of your questions, since a lot depends on your individual circumstances. Please be sure to ask your surgeon if there is anything you don’t understand about the procedure.
THE BEST CANDIDATES FOR BREAST RECONSTRUCTION
Most mastectomy patients are medically appropriate for reconstruction, many at the same time that the breast is removed. The best candidates, however, are women whose cancer, as far as can be determined, seems to have been eliminated by mastectomy.
Still, there are legitimate reasons to wait. Many women aren’t comfortable weighing all the options while they’re struggling to cope with a diagnosis of cancer. Others simply don’t want to have any more surgery than is absolutely necessary. Some patients may be advised by their surgeons to wait, particularly if the breast is being rebuilt in a more complicated procedure using flaps of skin and underlying tissue. Women with other health conditions, such as obesity, high blood pressure, or smoking, may also be advised to wait.
In any case, being informed of your reconstruction options before surgery can help you prepare for a mastectomy with a more positive outlook for the future.
ALL SURGERY CARRIES SOME UNCERTAINTY AND RISK
Virtually any woman who must lose her breast to cancer can have it rebuilt through reconstructive surgery. But there are risks associated with any surgery and specific complications associated with this procedure.
In general, the usual problems of surgery, such as bleeding, fluid collection, excessive scar tissue, or difficulties with anesthesia, can occur although they’re relatively uncommon. And, as with any surgery, smokers should be advised that nicotine can delay healing, resulting in conspicuous scars and prolonged recovery. Occasionally, these complications are severe enough to require a second operation.
If an implant is used, there is a remote possibility that an infection will develop, usually within the first two weeks following surgery. In some of these cases, the implant may need to be removed for several months until the infection clears. A new implant can later be inserted.
The most common problem, capsular contracture, occurs if the scar or capsule around the implant begins to tighten. This squeezing of the soft implant can cause the breast to feel hard. Capsular contracture can be treated in several ways, and sometimes requires either removal or “scoring” of the scar tissue, or perhaps removal or replacement of the implant.
Reconstruction has no known effect on the recurrence of disease in the breast, nor does it generally interfere with chemotherapy or radiation treatment, should cancer recur. Your surgeon may recommend continuation of periodic mammograms on both the reconstructed and the remaining normal breast. If your reconstruction involves an implant, be sure to go to a radiology center where technicians are experienced in the special techniques required to get a reliable x-ray of a breast reconstructed with an implant.
Women who postpone reconstruction may go through a period of emotional readjustment. Just as it took time to get used to the loss of a breast, a woman may feel anxious and confused as she begins to think of the reconstructed breast as her own.
PLANNING YOUR SURGERY
You can begin talking about reconstruction as soon as you’re diagnosed with cancer. Ideally, you’ll want your breast surgeon and your plastic surgeon to work together to develop a strategy that will put you in the best possible condition for reconstruction.
After evaluating your health, your surgeon will explain which reconstructive options are most appropriate for your age, health, anatomy, tissues, and goals. Be sure to discuss your expectations frankly with your surgeon. He or she should be equally frank with you, describing your options and the risks and limitations of each. Post-mastectomy reconstruction can improve your appearance and renew your self-confidence, but keep in mind that the desired result is improvement, not perfection.
Your surgeon should also explain the anesthesia he or she will use, the facility where the surgery will be performed, and the costs. In most cases, health insurance policies will cover most or all of the cost of post-mastectomy reconstruction. Check your policy to make sure you’re covered and to see if there are any limitations on what types of reconstruction are covered.
PREPARING FOR YOUR SURGERY
Your oncologist and your plastic surgeon will give you specific instructions on how to prepare for surgery, including guidelines on eating and drinking, smoking, and taking or avoiding certain vitamins and medications.
While making preparations, be sure to arrange for someone to drive you home after your surgery and to help you out for a few days, if needed.
WHERE YOUR SURGERY WILL BE PERFORMED
Breast reconstruction usually involves more than one operation. The first stage, whether done at the same time as the mastectomy or later on, is usually performed in a hospital.
Follow-up procedures may also be done in the hospital. Or, depending on the extent of surgery required, your surgeon may prefer an outpatient facility.
TYPES OF ANESTHESIA
The first stage of reconstruction, creation of the breast mound, is almost always performed using general anesthesia, so you’ll sleep through the entire operation.
Follow-up procedures may require only a local anesthesia, combined with a sedative to make you drowsy. You’ll be awake but relaxed, and may feel some discomfort.
TYPES OF IMPLANTS
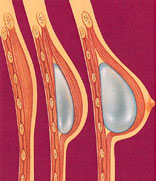
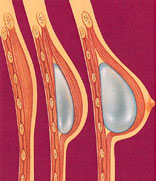
If your surgeon recommends the use of an implant, you’ll want to discuss what type of implant should be used. A breast implant is a silicone shell filled with either silicone gel or a salt-water solution known as saline.
Because of concerns that there is insufficient information demonstrating the safety of silicone gel-filled breast implants, the Food & Drug Administration (FDA) has determined that new gel-filled implants should be available only to women participating in approved studies. This currently includes women who already have tissue expanders (see below under Skin Expansion), who choose immediate reconstruction after mastectomy, or who already have a gel-filled implant and need it replaced for medical reasons. Eventually, all patients with appropriate medical indications may have similar access to silicone gel-filled implants.
The alternative saline-filled implant, a silicone shell filled with salt water, continues to be available on an unrestricted basis, pending further FDA review.
As more information becomes available, these FDA guidelines may change. Be sure to discuss current options with your surgeon.
THE SURGERY
While there are many options available in post-mastectomy reconstruction, you and your surgeon should discuss the one that’s best for you.
Skin expansion is the most common technique and is usually combined with subsequent insertion of an implant.
Following mastectomy, your surgeon will insert a balloon expander beneath your skin and chest muscle. Through a tiny valve mechanism buried beneath the skin, he or she will periodically inject a salt-water solution to gradually fill the expander over several weeks or months. After the skin over the breast area has stretched enough, the expander may be removed in a second operation and a more permanent implant will be inserted. Some expanders are designed to be left in place as the final implant. The nipple and the dark skin surrounding it, called the areola, are reconstructed in a subsequent procedure.
Some patients do not require preliminary tissue expansion before receiving an implant. For these women, the surgeon will proceed with inserting an implant as the first step.
Flap reconstruction. An alternative approach to implant reconstruction involves creation of a skin flap using tissue taken from other parts of the body, such as the back, abdomen, or buttocks.
In one type of flap surgery, the tissue remains attached to its original site, retaining its blood supply. The flap, consisting of the skin, fat, and muscle with its blood supply, are tunneled beneath the skin to the chest, creating a pocket for an implant or, in some cases, creating the breast mound itself, without need for an implant.
Another flap technique uses tissue that is surgically removed from the abdomen, thighs, or buttocks and then transplanted to the chest by reconnecting the blood vessels to new ones in that region. This procedure requires the skills of a plastic surgeon who is experienced in microvascular surgery as well.
Regardless of whether the tissue is tunneled beneath the skin on a pedicle or transplanted to the chest as a microvascular flap, this type of surgery is more complex than skin expansion. Scars will be left at both the tissue donor site and at the reconstructed breast, and recovery will take longer than with an implant. On the other hand, when the breast is reconstructed entirely with your own tissue, the results are generally more natural and there are no concerns about a silicone implant. In some cases, you may have the added benefit of a improved abdominal contour.
Follow-up procedures. Most breast reconstruction involves a series of procedures that occur over time. Usually, the initial reconstructive operation is the most complex. Follow-up surgery may be required to replace a tissue expander with an implant or to reconstruct the nipple and the areola. Many surgeons recommend an additional operation to enlarge, reduce, or lift the natural breast to match the reconstructed breast. But keep in mind, this procedure may leave scars on an otherwise normal breast and may not be covered by insurance.
AFTER YOUR SURGERY
You are likely to feel tired and sore for a week or two after reconstruction. Most of your discomfort can be controlled by medication prescribed by your doctor.
Depending on the extent of your surgery, you’ll probably be released from the hospital in two to five days. Many reconstruction options require a surgical drain to remove excess fluids from surgical sites immediately following the operation, but these are removed within the first week or two after surgery. Most stitches are removed in a week to 10 days.
GETTING BACK TO NORMAL
It may take you up to six weeks to recover from a combined mastectomy and reconstruction or from a flap reconstruction alone. If implants are used without flaps and reconstruction is done apart from the mastectomy, your recovery time may be less.
Reconstruction cannot restore normal sensation to your breast, but in time, some feeling may return. Most scars will fade substantially over time, though it may take as long as one to two years, but they’ll never disappear entirely. The better the quality of your overall reconstruction, the less distracting you’ll find those scars.
Follow your surgeon’s advice on when to begin stretching exercises and normal activities. As a general rule, you’ll want to refrain from any overhead lifting, strenuous sports, and sexual activity for three to six weeks following reconstruction.
YOUR NEW LOOK
Chances are your reconstructed breast may feel firmer and look rounder or flatter than your natural breast. It may not have the same contour as your breast before mastectomy, nor will it exactly match your opposite breast. But these differences will be apparent only to you. For most mastectomy patients, breast reconstruction dramatically improves their appearance and quality of life following surgery.
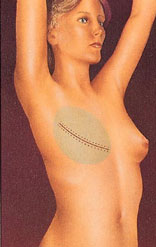
A tissue expander is inserted following the mastectomy to prepare for reconstruction.
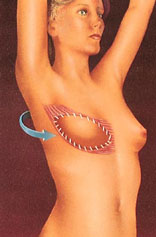
The expander is gradually filled with saline through an integrated or separate tube to stretch the skin enough to accept an implant beneath the chest muscle.
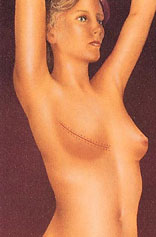
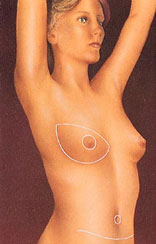
After surgery, the breast mound is restored. Scars are permanent, but will fade with time. The nipple and areola are reconstructed at a later date.
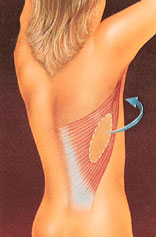
With flap surgery, tissue is taken from the back and tunneled to the front of the chest wall to support the reconstructed breast.
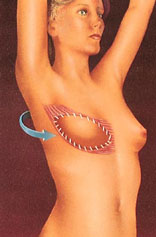
The transported tissue forms a flap for a breast implant, or it may provide enough bulk to form the breast mound without an implant.

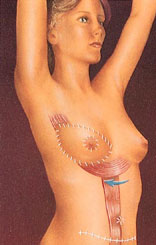
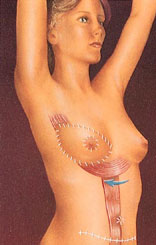
Tissue may be taken from the abdomen and tunneled to the breast or surgically transplanted to form a new breast mound.
After surgery, the breast mound, nipple, and areola are restored.
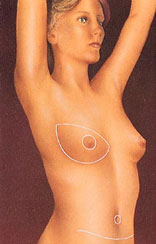
Scars at the breast, nipple, and abdomen will fade substantially with time, but may never disappear entirely.
Breast
Breast Reconstruction Procedures
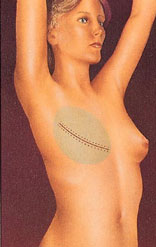
A tissue expander is inserted following the mastectomy to prepare for reconstruction.
The expander is gradually filled with saline through an integrated or separate tube to stretch the skin enough to accept an implant beneath the chest muscle.
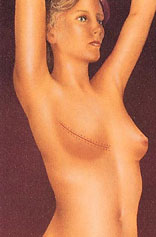
After surgery, the breast mound is restored. Scars are permanent, but will fade with time. The nipple and areola are reconstructed at a later date.
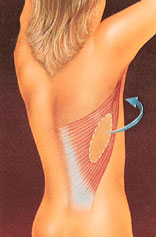
With flap surgery, tissue is taken from the back and tunneled to the front of the chest wall to support the reconstructed breast.
The transported tissue forms a flap for a breast implant, or it may provide enough bulk to form the breast mound without an implant.

Tissue may be taken from the abdomen and tunneled to the breast or surgically transplanted to form a new breast mound.
After surgery, the breast mound, nipple, and areola are restored.
Scars at the breast, nipple, and abdomen will fade substantially with time, but may never disappear entirely.
IF YOU ARE CONSIDERING BREAST RECONSTRUCTION…
Reconstruction of a breast that has been removed due to cancer or other disease is one of the most rewarding surgical procedures available today. New medical techniques and devices have made it possible for surgeons to create a breast that can come close in form and appearance to matching a natural breast. Frequently, reconstruction is possible immediately following breast removal (mastectomy), so the patient wakes up with a breast mound already in place, having been spared the experience of seeing herself with no breast at all.
But bear in mind, post-mastectomy breast reconstruction is not a simple procedure. There are often many options to consider as you and your doctor explore what’s best for you.
This information will give you a basic understanding of the procedure, when it’s appropriate, how it’s done, and what results you can expect. It can’t answer all of your questions, since a lot depends on your individual circumstances. Please be sure to ask your surgeon if there is anything you don’t understand about the procedure.
THE BEST CANDIDATES FOR BREAST RECONSTRUCTION
Most mastectomy patients are medically appropriate for reconstruction, many at the same time that the breast is removed. The best candidates, however, are women whose cancer, as far as can be determined, seems to have been eliminated by mastectomy.
Still, there are legitimate reasons to wait. Many women aren’t comfortable weighing all the options while they’re struggling to cope with a diagnosis of cancer. Others simply don’t want to have any more surgery than is absolutely necessary. Some patients may be advised by their surgeons to wait, particularly if the breast is being rebuilt in a more complicated procedure using flaps of skin and underlying tissue. Women with other health conditions, such as obesity, high blood pressure, or smoking, may also be advised to wait.
In any case, being informed of your reconstruction options before surgery can help you prepare for a mastectomy with a more positive outlook for the future.
ALL SURGERY CARRIES SOME UNCERTAINTY AND RISK
Virtually any woman who must lose her breast to cancer can have it rebuilt through reconstructive surgery. But there are risks associated with any surgery and specific complications associated with this procedure.
In general, the usual problems of surgery, such as bleeding, fluid collection, excessive scar tissue, or difficulties with anesthesia, can occur although they’re relatively uncommon. And, as with any surgery, smokers should be advised that nicotine can delay healing, resulting in conspicuous scars and prolonged recovery. Occasionally, these complications are severe enough to require a second operation.
If an implant is used, there is a remote possibility that an infection will develop, usually within the first two weeks following surgery. In some of these cases, the implant may need to be removed for several months until the infection clears. A new implant can later be inserted.
The most common problem, capsular contracture, occurs if the scar or capsule around the implant begins to tighten. This squeezing of the soft implant can cause the breast to feel hard. Capsular contracture can be treated in several ways, and sometimes requires either removal or “scoring” of the scar tissue, or perhaps removal or replacement of the implant.
Reconstruction has no known effect on the recurrence of disease in the breast, nor does it generally interfere with chemotherapy or radiation treatment, should cancer recur. Your surgeon may recommend continuation of periodic mammograms on both the reconstructed and the remaining normal breast. If your reconstruction involves an implant, be sure to go to a radiology center where technicians are experienced in the special techniques required to get a reliable x-ray of a breast reconstructed with an implant.
Women who postpone reconstruction may go through a period of emotional readjustment. Just as it took time to get used to the loss of a breast, a woman may feel anxious and confused as she begins to think of the reconstructed breast as her own.
PLANNING YOUR SURGERY
You can begin talking about reconstruction as soon as you’re diagnosed with cancer. Ideally, you’ll want your breast surgeon and your plastic surgeon to work together to develop a strategy that will put you in the best possible condition for reconstruction.
After evaluating your health, your surgeon will explain which reconstructive options are most appropriate for your age, health, anatomy, tissues, and goals. Be sure to discuss your expectations frankly with your surgeon. He or she should be equally frank with you, describing your options and the risks and limitations of each. Post-mastectomy reconstruction can improve your appearance and renew your self-confidence, but keep in mind that the desired result is improvement, not perfection.
Your surgeon should also explain the anesthesia he or she will use, the facility where the surgery will be performed, and the costs. In most cases, health insurance policies will cover most or all of the cost of post-mastectomy reconstruction. Check your policy to make sure you’re covered and to see if there are any limitations on what types of reconstruction are covered.
PREPARING FOR YOUR SURGERY
Your oncologist and your plastic surgeon will give you specific instructions on how to prepare for surgery, including guidelines on eating and drinking, smoking, and taking or avoiding certain vitamins and medications.
While making preparations, be sure to arrange for someone to drive you home after your surgery and to help you out for a few days, if needed.
WHERE YOUR SURGERY WILL BE PERFORMED
Breast reconstruction usually involves more than one operation. The first stage, whether done at the same time as the mastectomy or later on, is usually performed in a hospital.
Follow-up procedures may also be done in the hospital. Or, depending on the extent of surgery required, your surgeon may prefer an outpatient facility.
TYPES OF ANESTHESIA
The first stage of reconstruction, creation of the breast mound, is almost always performed using general anesthesia, so you’ll sleep through the entire operation.
Follow-up procedures may require only a local anesthesia, combined with a sedative to make you drowsy. You’ll be awake but relaxed, and may feel some discomfort.
TYPES OF IMPLANTS
If your surgeon recommends the use of an implant, you’ll want to discuss what type of implant should be used. A breast implant is a silicone shell filled with either silicone gel or a salt-water solution known as saline.
Because of concerns that there is insufficient information demonstrating the safety of silicone gel-filled breast implants, the Food & Drug Administration (FDA) has determined that new gel-filled implants should be available only to women participating in approved studies. This currently includes women who already have tissue expanders (see below under Skin Expansion), who choose immediate reconstruction after mastectomy, or who already have a gel-filled implant and need it replaced for medical reasons. Eventually, all patients with appropriate medical indications may have similar access to silicone gel-filled implants.
The alternative saline-filled implant, a silicone shell filled with salt water, continues to be available on an unrestricted basis, pending further FDA review.
As more information becomes available, these FDA guidelines may change. Be sure to discuss current options with your surgeon.
THE SURGERY
While there are many options available in post-mastectomy reconstruction, you and your surgeon should discuss the one that’s best for you.
Skin expansion is the most common technique and is usually combined with subsequent insertion of an implant.
Following mastectomy, your surgeon will insert a balloon expander beneath your skin and chest muscle. Through a tiny valve mechanism buried beneath the skin, he or she will periodically inject a salt-water solution to gradually fill the expander over several weeks or months. After the skin over the breast area has stretched enough, the expander may be removed in a second operation and a more permanent implant will be inserted. Some expanders are designed to be left in place as the final implant. The nipple and the dark skin surrounding it, called the areola, are reconstructed in a subsequent procedure.
Some patients do not require preliminary tissue expansion before receiving an implant. For these women, the surgeon will proceed with inserting an implant as the first step.
Flap reconstruction. An alternative approach to implant reconstruction involves creation of a skin flap using tissue taken from other parts of the body, such as the back, abdomen, or buttocks.
In one type of flap surgery, the tissue remains attached to its original site, retaining its blood supply. The flap, consisting of the skin, fat, and muscle with its blood supply, are tunneled beneath the skin to the chest, creating a pocket for an implant or, in some cases, creating the breast mound itself, without need for an implant.
Another flap technique uses tissue that is surgically removed from the abdomen, thighs, or buttocks and then transplanted to the chest by reconnecting the blood vessels to new ones in that region. This procedure requires the skills of a plastic surgeon who is experienced in microvascular surgery as well.
Regardless of whether the tissue is tunneled beneath the skin on a pedicle or transplanted to the chest as a microvascular flap, this type of surgery is more complex than skin expansion. Scars will be left at both the tissue donor site and at the reconstructed breast, and recovery will take longer than with an implant. On the other hand, when the breast is reconstructed entirely with your own tissue, the results are generally more natural and there are no concerns about a silicone implant. In some cases, you may have the added benefit of a improved abdominal contour.
Follow-up procedures. Most breast reconstruction involves a series of procedures that occur over time. Usually, the initial reconstructive operation is the most complex. Follow-up surgery may be required to replace a tissue expander with an implant or to reconstruct the nipple and the areola. Many surgeons recommend an additional operation to enlarge, reduce, or lift the natural breast to match the reconstructed breast. But keep in mind, this procedure may leave scars on an otherwise normal breast and may not be covered by insurance.
AFTER YOUR SURGERY
You are likely to feel tired and sore for a week or two after reconstruction. Most of your discomfort can be controlled by medication prescribed by your doctor.
Depending on the extent of your surgery, you’ll probably be released from the hospital in two to five days. Many reconstruction options require a surgical drain to remove excess fluids from surgical sites immediately following the operation, but these are removed within the first week or two after surgery. Most stitches are removed in a week to 10 days.
GETTING BACK TO NORMAL
It may take you up to six weeks to recover from a combined mastectomy and reconstruction or from a flap reconstruction alone. If implants are used without flaps and reconstruction is done apart from the mastectomy, your recovery time may be less.
Reconstruction cannot restore normal sensation to your breast, but in time, some feeling may return. Most scars will fade substantially over time, though it may take as long as one to two years, but they’ll never disappear entirely. The better the quality of your overall reconstruction, the less distracting you’ll find those scars.
Follow your surgeon’s advice on when to begin stretching exercises and normal activities. As a general rule, you’ll want to refrain from any overhead lifting, strenuous sports, and sexual activity for three to six weeks following reconstruction.
YOUR NEW LOOK
Chances are your reconstructed breast may feel firmer and look rounder or flatter than your natural breast. It may not have the same contour as your breast before mastectomy, nor will it exactly match your opposite breast. But these differences will be apparent only to you. For most mastectomy patients, breast reconstruction dramatically improves their appearance and quality of life following surgery.
